Portal Hypertension
What is portal hypertension?
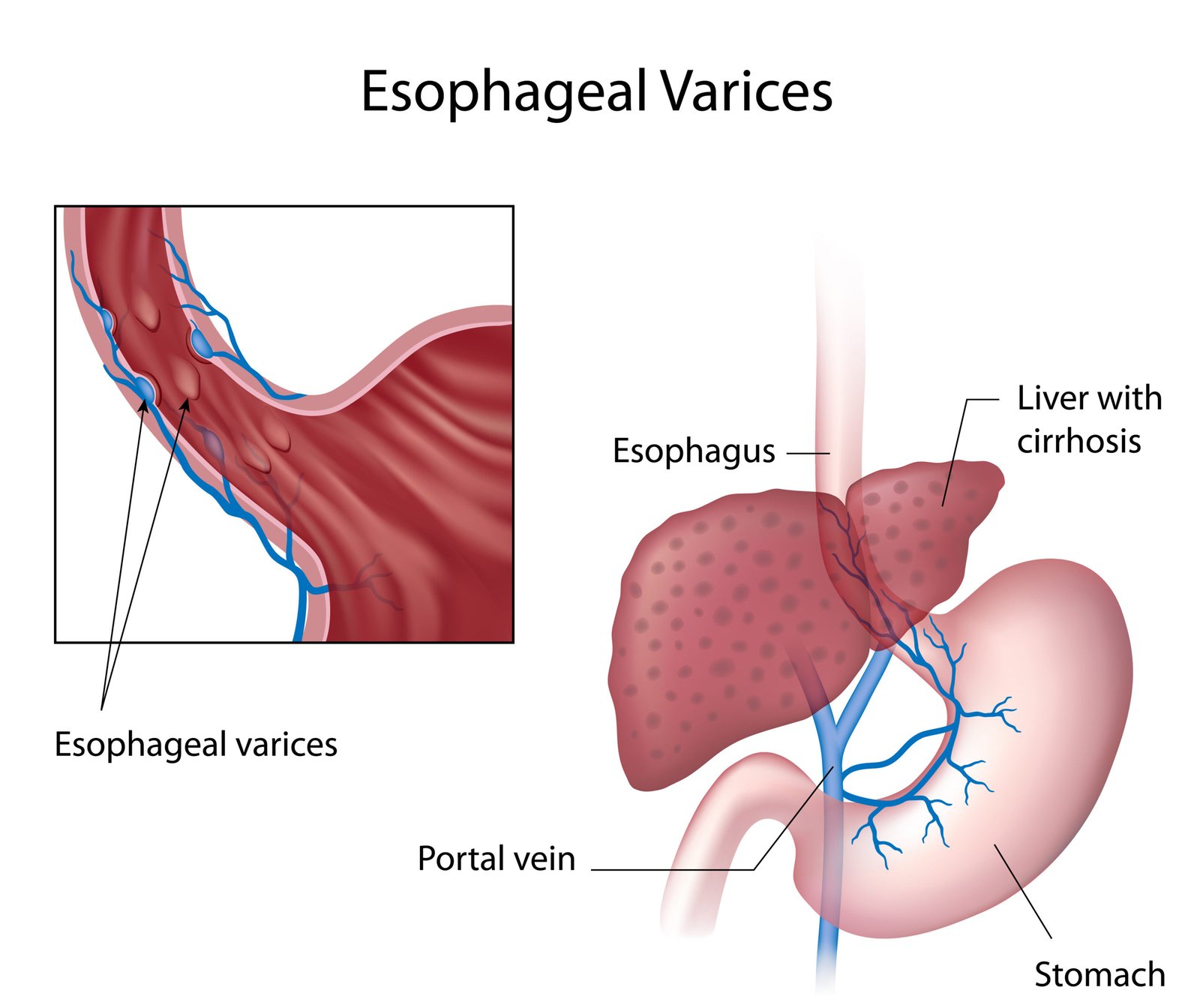
Portal hypertension refers to an increase in pressure within the vein that carries blood to the liver from the digestive organs (the portal vein). A blockage in the liver's blood flow is the cause of portal hypertension, which can result in varices (large veins) developing across the stomach and oesophagus, as a way for the body to circumnavigate the blockage. These large veins are fragile and susceptible to bleeding.
What causes portal hypertension?
The scarring of the liver (cirrhosis) is typically the cause of portal hypertension. Cirrhosis is the result of healing from liver injury which has been caused by alcohol abuse, hepatitis or another source of liver damage. Cirrhosis involves the blocking of the blood flow by scar tissue in the liver, and this can lead to the slowing of the liver's processing functions.
Thrombosis and blood clots are other potential causes of hypertension.
Symptoms of portal hypertension
Portal hypertension does not always produce symptoms that can indicate a liver problem. However, people with liver disease that has resulted in cirrhosis have a high chance of portal hypertension.
The predominant symptoms of portal hypertension can include; fluid accumulating in the abdomen (ascites); gastrointestinal bleeding indicated by vomiting blood or black stools; a reduced white blood cell count; a reduced level of platelets in the blood; and forgetfulness or confusion caused by the blood flow being diverted away from the liver and the poor function of the liver (encephalopathy).
Treatment options for portal hypertension
Portal hypertension can be diagnosed via; imaging tests such as x-ray, an endoscopic examination, and lab tests to check for variceal bleeding.
Once a diagnosis of portal hypertension has been made, there are a number of treatment options available:
Endoscopic therapy and medications can be recommended as the first line of treatment if you have variceal bleeding. Endoscopic therapy will be either banding or sclerotherapy; banding involves a gastroenterologist blocking the blood supply to each enlarged vein using rubber bands; sclerotherapy involves the injection of a solution into bleeding veins to control bleeding.
Medications prescribed can include beta-blockers, nitrates, propranolol and isosorbide.
Changes to lifestyle and diet can help the liver to function properly. People with portal hypertension could be advised to stop drinking alcohol or taking any recreational drugs, and stick to a diet that is low in salt.
If the treatments outlined above have been unsuccessful in controlling variceal bleeding, a decompression procedure may be required in order to reduce the pressure.
Transjugular intrahepatic portosystemic shunt (TIPS) involves the placement of a tubular device (stent) in the liver, and a distal splenorenal shunt (DSRS) is a procedure to connect the left kidney with the splenic vein, controlling bleeding and reducing the pressure in the varices.
Other treatment options for portal hypertension include; devascularisation, a procedure to remove bleeding varices that can be done when TIPS or DSRS is not possible; a liver transplant; or the removal of fluid build up in the abdomen via a paracentesis.
